
Skin Cancer checks and mole surveillance
Dr Lee is known for his skills in the early detection and management of pre-cancerous lesions and skin cancers. Dr Lee will inspect your skin using an instrument called a dermatoscope, which allows him to view the subtle features on your skin. During your skin check, Dr Lee will also take the time to educate you on what to look out for. At Laye Dermatology, Dr Lee uses state of the art body mapping software that allows serial dermatoscopic monitoring of any skin lesions. This ensures that on subsequent skin examinations, any change in a lesion is detected early. An annual skin check is advised, however patients who are at higher risk such as a personal history of skin cancers or have been diagnosed with a malignant melanoma may be seen more frequently. Dr Lee will guide you through your treatment options in the management of your skin cancers.
Actinic keratoses
Actinic keratoses (sunspots) are precancerous lesions caused by exposure to ultraviolet (UV) radiation. A proportion of actinic keratoses if left untreated may progress to skin cancer known as a squamous cell carcinoma. Actinic keratoses may appear as flat or thickened areas of red or pigmented scaly skin. They may sometimes be sensitive or tender. The presence of actinic keratoses is an indication of sun damage to your skin and so other signs of sun damage such as pigmentation, broken capillaries and fine lines may be present.
The type of treatment for your actinic keratoses will depend on the nature, number and location. Cryotherapy or liquid nitrogen therapy may be used to freeze the damaged cells.
If you have a number of sunspots, then “field treatment” may be more appropriate. Field treatment involves treating a whole area such as the entire face to achieve a more uniform and improved result. Field treatment may be in the form of a cream called 5-Fluoruracil which is a chemotherapy medication. This is a chemical way of removing the sun damaged skin cells. Alternatively, a laser peel which physically removes the abnormal cells in the top layer of the skin called the epidermis may be used. A laser peel is a more wholistic approach to photorejuvenation which aims to address all the facets of sun damage.


Basal Cell Carcinoma
Basal cell carcinoma (BCC) is the most common skin cancer worldwide. Basal cell carcinomas are caused by environmental factors including sunlight and genetic factors. There are different variants of BCCs, which reflects the biological behaviour of the cancer. If left untreated BCCs will grow and cause local structural damage and disfigurement. Sometimes a diagnosis of a BCC may require a biopsy. Basal cell carcinomas may be treated with topical creams, standard surgical excision or Mohs micrographic surgery. Dr Lee will discuss with you your treatment options, which will depend on the variant you have, location, size and medical history.
Squamous cell carcinoma
Squamous cell carcinomas (SCC) are the second most common skin cancer in Australia. Ultraviolet radiation from the sun is a common risk factor for developing SCCs. Other risk factors include a supressed immune system, sites of previous injury such as a burn or radiation, or a viral infection such as the human papilloma virus (HPV). Squamous cell carcinomas may arise from a pre-existing actinic keratosis (sunspot). An SCC that is confined to the top layer of the skin (epidermis) is called Bowen’s disease. When the tumour cells break away from the epidermis, then it is known as an invasive SCC. If left untreated, squamous cell carcinomas can potentially spread to the lymph nodes and internal organs. Sometimes a diagnosis of an SCC may require a biopsy. Squamous cell carcinomas may be treated with topical creams, standard surgical excision or Mohs micrographic surgery. Dr Lee will discuss with you your treatment options, which will depend on the variant you have, location, size and medical history.


Malignant melanoma
Malignant melanoma is a serious type of skin cancer that if left untreated is life-threatening. Australia and New Zealand have the highest incidence of malignant melanoma.
Within the skin there are normal pigment cells called melanocytes, which gives our natural skin colour and also form the moles (naevi) on our body. When the melanocytes undergo cancerous change then it is known as a malignant melanoma. The development of malignant melanoma is influenced by both environmental and genetic factors. Dr Lee will ask you whether there is a family history as this is often useful in identifying those at risk.
Malignant melanomas can arise as a new spot on your skin or from an existing mole that has recently changed. It is important to tell your dermatologist about any new or changing moles. A biopsy is necessary to make a diagnosis of malignant melanoma. The treatment is dependent on the stage and type of malignant melanoma. Early stage melanomas are usually successfully treated with standard surgical excision. Dr Lee will make the most appropriate plan of management for you malignant melanoma.
Acne and acne scarring
Acne is a common inflammatory condition that affects up to 85% of the adolescent population, although it can be observed in patients of all ages. The cause of acne is multifactorial. Genetics, hormones, bacteria, psychological stress and diet all contribute to acne production. Acne may present as whiteheads and blackheads (comedonal acne), pustules or deep-seated cysts. It is important to treat acne early as this minimises discolouration and potential life-long scarring which can be detrimental to ones self-esteem. The treatment of acne includes anti-bacterial washes, prescriptive gels and lotions, hormonal therapy, prescriptive oral medications or broad band light therapy (BBL).
Broad band light therapy uses a combination of blue, yellow, and infrared light to eliminate bacteria, reduce inflammation, and promote the body’s natural healing process to clear acne. During a BBL treatment, patients feel minimal discomfort as the BBL handpiece gently glides across the skin. The treatment involves several passes of the device over the treatment area. The first pass uses blue light to eliminate acne-causing bacteria located deep within the skin’s pores. The second pass uses yellow light to reduce inflammation and acne-associated redness while preventing new breakouts. To maximize patients’ results, the skin receives a third pass using infra-red light in rapid, gentle pulses to initiate the body’s natural healing process, reduce the appearance of existing scars, and enhance the benefits of the first two steps. You should feel minimal to no discomfort during treatment as the BBL handpiece gently glides across the skin. A sapphire at the tip of the BBL applicator keeps the skin cool and comfortable throughout the treatment. Afterward, most patients will continue to feel warm for 30 to 60 minutes.
Dr Lee will customise your acne treatment plan tailored to meet your specific needs.


Rosacea
Rosacea is a common skin condition that presents as red bumps, pustules, broken capillaries, generalised facial redness or a combination thereof. Rosacea can also affect the eyelids and present as irritated eyes. Rosacea occurs mostly in fair skinned individuals and is a chronic relapsing, remitting disorder. There are several causes for rosacea, which includes hyperactive blood vessels in the skin or infestation with the demodex mite. There are several trigger factors including sunlight, heat, alcoholic beverages, spicy foods and caffeine.
The treatment of rosacea is dependent on the variant you have. The bumps and pustules respond better to prescriptive oral medications and creams. The facial redness may be treated with a series of broad band light (BBL) and vascular laser treatments.
The light that is released from the BBL which strikes the target tissue is more attracted to certain chromophores or skin pigments. There are basically three chromophores in the skin which are targets when treating with BBL light; haemoglobin (redness), melanin (brown) and water. The aim of BBL treatment is reduction and improvement of redness and/or pigmentation. The vascular laser selectively targets haemoglobin and deposits heat into blood vessels. This heat increases the temperature of the blood that is flowing through the blood vessel. This in turn will heat the blood vessel wall causing it to collapse. The heating of the small blood vessels can also induce an inflammatory response causing the release of mediators that stimulate fibroblast cell activity and the body’s natural repair process resulting in COLLAGEN production.
You should feel minimal to no discomfort during treatment as the BBL handpiece gently glides across the skin. A sapphire at the tip of the BBL applicator keeps the skin cool and comfortable throughout the treatment. Afterward, most patients will continue to feel warm for 30 to 60 minutes. Patients typically can return to normal activities immediately following treatment with BBL and vascular laser.
You will require multiple treatment sessions depending on how much redness you have on your skin. Each treatment is generally performed every 4 weeks. Dr Lee will advise you on how many treatments are required.
Dr Lee will customise your rosacea treatment plan tailored to meet your specific needs.
Dermatitis
Dermatitis is a term that describes inflamed, itchy, scaly skin. Atopic dermatitis is a chronic relapsing remitting condition that may occur at any age but usually presents early in life. The causes of atopic dermatitis are both genetic and environmental. Unfortunately there is no cure for atopic dermatitis and it is a condition that is managed with soap substitutes, emollients, prescriptive creams and ointments and in severe cases phototherapy or oral medication.
There are new medications called Small Molecules and Biologics which are a class of immune modulators that may also control atopic dermatitis and can only be prescribed by a specialist dermatologist.


Psoriasis
Psoriasis is an inflammatory skin condition characterised by red, scaly plaques with well-defined edges and generally occurs symmetrically on the body. The usual sites include the knees and elbows, although any part of the body may be affected. The incidence of psoriasis is 2-4% and can occur early or later on in life. Genetics play an important role in the cause of psoriasis.
Psoriasis is a chronic relapsing remitting condition. Unfortunately there is no cure but it can be cleared and managed well with emollients, prescriptive creams and ointments and in severe cases phototherapy or oral medication. There are new medications called Small Molecules and Biologics which are a class of immune modulators that may also control psoriasis and can only be prescribed by a specialist dermatologist.
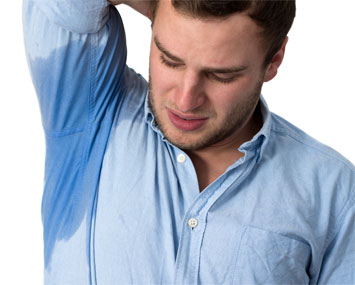
Excessive armpit sweating
Axillary hyperhidrosis (excessive armpit sweating) affects approximately 1.4% of the population. It can be embarrassing, debilitating and interfere with one’s daily life. Botulinum toxin injection is minimally invasive and has become the treatment of choice for those who fail other measures. Botulinum toxin works by blocking a neurotransmitter called acetylcholine that is responsible for turning on the sweat glands.
To help make the procedure as comfortable as possible, a numbing cream is applied to your armpit area prior to your injections. Small amounts are injected into or near the sweat glands, which usually takes 15 minutes. It may take up to three weeks to see the effects, which usually lasts up to seven months.
Dr Lee is an accredited axillary hyperhidrosis injector, which may attract a Medicare rebate.
Standard surgical excision
The area of concern is marked with a rim of normal tissue and excised under local anaesthesia. The lesion excised is then sent to the laboratory for testing. The hole that remains after the lesion has been removed is closed in layers with deep dissolving sutures and superficial skin sutures that require removal one to two weeks later. The pathology results usually takes about a week to come back.

Flaps
In some instances, it may not be possible to reconstruct the hole made after surgery with a standard surgical closure due to the anatomical site or if the surrounding skin has limited laxity. In such circumstances the hole may be closed with a flap, which requires an understanding of the three dimensional geometric movement of the surrounding skin.
Grafts
A graft is when skin is harvested from areas of similar colour and texture, which is then sutured into the hole made after surgery. The donor site is closed like a standard surgical excision. Once the graft is transplanted, it is secured into place with sutures and then it is covered with a special bolster dressing that is sutured into place. The graft relies on the blood supply and nutrients from the bed on which it is placed for survival. Therefore a lot of care and rest is required to provide the best opportunity for the graft to take and survive. The bolster dressing is left on for one to two weeks until you see the nurse for removal of sutures.
Mohs Micrographic Surgery
What is Mohs surgery?
Mohs surgery is a highly specialised technique for the removal of skin cancers such as basal cell carcinomas (BCC) and squamous cell carcinomas (SCC). The name Mohs refers to Dr Frederic Mohs, a dermatologist who pioneered this technique for removal of skin cancers. Some skin cancers are like an octopus; the head is easily seen with the naked eye however the “tentacles” which is not visible to the naked eye grows downwards and outwards into the skin. Mohs surgery allows these areas to be detected under a microscope and maximises the chance of cure.
What does Mohs surgery involve?
On the day of your surgery, Dr Lee will mark out the area of concern. Mohs surgery is performed under local anaesthetic. Once the area is numb, Dr Lee will remove the first layer, with its edges marked with coloured dyes and a map of the specimen is made. The tissue is then processed onto microscope slides in the laboratory. Dr Lee then reviews the slides under a microscope looking for any evidence of skin cancer. During this time, the area of concern will still be numb and have a dressing over it. You will be placed in a comfortable private area during this time. If Dr Lee identifies any cancers cells after he has taken the first layer, then an additional layer will be removed only in the area where the cancer cells have been detected, leaving normal healthy skin intact. This maximises your chances of cure and minimises removal of healthy normal skin.
Once the cancer has been fully removed, the wound may be closed with sutures in a side-side manner, or with a flap or graft. Dr Lee or a plastic and reconstructive surgeon may perform the second stage of closing the wound.
How long does Mohs surgery take?
While it may be difficult to predict, due to the nature of your skin cancer, Mohs surgery typically takes several hours.
My skin cancer is less evident after I have had the biopsy. Do I still need Mohs surgery?
Sometimes your skin cancer that has been biopsied may be less evident. This does not necessarily mean the cancer is all gone. The biopsy may represent the “octopus head” and the “tentacles” may still remain in the skin, which is just not visible to the naked eye. The residual cancer cells may give rise to daughter cells over time and re-appear sometime later, which may require more extensive surgery.

Laser and Light
Lasers and light therapies may be used to treat a host of dermatological conditions. There are many different lasers and light devices, each of which specifically target different anatomical structures in the skin. During your consultation, Dr Lee will assess your concerns and advise on the best type of laser or light therapy. Dr Lee will discuss with you what is involved in your treatment, side effects, downtime and expected results.
HEROic Broadband Light (BBL)
HEROic BBL energy can be used to treat the following conditions:
- Rosacea
- Acne
- Solar lentigines (brown sun spots)
- Telangiectasia (small facial veins)
- Angiomas (proliferation of blood vessels) such as spider naevi or cherry angiomas.
- Poikiloderma of Civatte
- Redness in scars
How does HEROic BBL work?
HEROic BBL is the first energy based device where AI ensures your treatment is accurately performed. This leads to better results and patient safety than standard IPL machines. The light or heat that is released from the HEROic BBL which strikes the target tissue is more attracted to certain chromophores or skin pigments. There are basically three chromophores in the skin which are targets when treating with HEROic BBL light; hemoglobin (redness), melanin (brown) and water. The aim of HEROic BBL treatment is reduction and improvement of redness and/or pigmentation.
You will require multiple treatment sessions depending on how much redness and pigmentation you have in your skin. Your doctor will advise you on how many treatments is required.
Each HEROic BBL treatment is generally performed every 4-6 weeks.


Vascular Laser
Vascular laser can be used to treat the following conditions:
- Rosacea
- Acne
- Poikiloderma of Civatte
- Port Wine Stains
- Cherry angiomas
- Spider angiomas
- Venous lakes
- Fine lines
- Appearance of pores
- Uneven skin texture
- Scars
How does the vascular laser work?
The vascular laser selectively targets haemoglobin and deposits heat into blood vessels. This heat increases the temperature of the blood that is flowing through the blood vessel. This in turn will heat the blood vessel wall causing it to collapse.
The heating of the small vessels can also induce an inflammatory response causing the release of mediators that stimulate fibroblast cell activity and the body’s natural repair process resulting in collagen production.
You may require multiple treatment sessions depending on how much redness and fine lines you have on your skin. Your doctor will advise you on how many treatments is required.
Each vascular laser treatment is generally performed every 4 weeks.
Hybrid Fractional Laser
The Hybrid Fractional Laser combines the best attributes of both non-ablative and ablative fractional lasers. It is used for the treatment of:
- UVR damage – actinic keratoses also known as sunspots
- Pigmentation
- Dull skin tone
- Enlarged pores
- Scars
- Fine lines
How does the Hybrid Fractional Laser work?
The Hybrid Fractional Laser laser creates columns of injury to the skin called microscopic thermal zones (MTZs). This causes ablation (peeling) of the outer layer of the skin called the epidermis and coagulates (heats) the collagen in the second layer of the skin called the dermis. This process has two effects:
- Expels the sun damaged cells in the epidermis.
- Activates a molecule called Activator Protein 1 (AP-1) transcription factor which leads to upregulation of matrix metalloproteinase (MMPs) which stimulates collagen remodelling.


Erbium Yag Laser Peel
The Ablative Erbium-Yag laser is a fully ablative laser that precisely removes layers of the skin. It incorporates the Nanolaser Peel, Microlaser Peel and Deep Resurfacing laser. It is used for the treatment of:
- UVR damage to the skin called actinic keratoses also known as sunspots
- UVR damage to the lip called actinic cheilitis
- Seborrhoeic keratoses also known as pigmented spots
- Debulking of benign tumours
- Scars
- Warts
- Rhytides (lines)
- Enlarged pores
How does the Ablative Erbium-Yag laser work?
The Ablative Erbium-Yag laser fully ablates (peels) the skin from the outer layer of the skin called the epidermis to the deeper layer of the skin called the dermis. The Ablative Erbium-Yag laser also has the ability to coagulate (heat) the collagen in the dermis. This process has two effects:
- Expels the sun damaged cells in the epidermis and dermis.
- Activates a molecule called Activator Protein 1 (AP-1) transcription factor which leads to upregulation of matrix metalloproteinase (MMPs) which stimulates collagen remodelling.
Profractional Erbium Yag Laser
The Profractional laser is an ablative fractional laser. It is used for the treatment of:
- UVR damage – actinic keratoses also known as sunspots
- Scars
- Rhytides (lines)
- Enlarged pores
How does the Profractional laser work?
The Profractional laser creates columns of injury to the skin called microscopic treatment zones (MTZs) covering a fraction of the total surface area. This causes ablation (peeling) of the skin from the outer layer of the skin called the epidermis to the deeper layer of the skin called the dermis. The Profractional laser also has the ability to coagulate (heat) the collagen in the dermis. This process has two effects:
- Expels the sun damaged cells in the epidermis and dermis.
- Activates a molecule called Activator Protein 1 (AP-1) transcription factor which leads to upregulation of matrix metalloproteinase (MMPs) which stimulates collagen remodelling.






